
Created by Khang Hee Gan, July 2021
Back to topicsKetamine Accreditation in Starship CED
Ketamine is a commonly used drug for procedural sedation in CED.
In order to achieve ketamine accreditation in CED, you will be required to complete these 2 components:
1. Complete the Ketamine Module: Please read the notes provided and complete the MCQ (link present at the end of the notes). You will need to achieve 8 or more correct answers (out of 10 questions) to pass this component. You can re-sit this MCQ as many times as you want – just remember to enter your email address and name prior to starting the MCQ.
2. Complete the Ketamine Sign-Off:
A. If you have previously achieved ketamine accreditation for procedural sedation in children (either in CED or in another emergency department), you are required to successfully pass these requirements:
· RACP trainees: Observe one ketamine sedation, then do one directly supervised ketamine sedation (supervised by SMO)
· ACEM trainees: one directly supervised ketamine sedation (supervised by SMO) done as a formal DOPS (direct observation of procedural skills)
B. If you have not previously achieved ketamine accreditation for procedural sedation in children, you are required to:
· Observe one ketamine sedation
· Do two directly supervised ketamine sedation (supervised by SMO)
· Do three indirectly supervised ketamine sedation (supervised by SMO)
Finally, one final supervised ketamine sedation (supervised by SMO) before being “signed off”.
The ketamine sign off sheet is located in Procedure room 2 in CED.
Introduction
- Ketamine is a synthetic phencyclidine derivative that causes a dissociative sedative state through binding with the NMDA (N-methyl-D-aspartate) receptor.
- Characteristics of ketamine “dissociative state”:
- Dissociation: trance-like state – eyes remain open, but patient does not respond
- Catalepsy: normal or slightly increased muscle tone; occasional muscular clonus may occur
- Anxiolysis
- Analgesia (substantial or complete)
- Amnesia (total)
- Maintenance of protective airway reflexes
- Cardiovascular stability: heart rate and blood pressure typically increase
- Nystagmus
- Dissociation from ketamine is either present or absent, with a narrow transition zone, and has no observable progression or depth, therefore further dosing does not cause deeper sedation.
- Ketamine has a wide margin of safety.
- The ketamine doses advised for procedural sedation are designed to leave the patient capable of maintaining their airway. There is a significant risk of failure of sedation if the procedure is prolonged. If a procedure is likely to be longer than 20 minutes, a general anaesthesia should be considered as an alternative.
- Ketamine onset:
- Clinical onset (approximately) 1 minute
- Effective sedation 10 – 20 minutes
- Time to discharge 90 minutes
- Ketamine should be used to facilitate short painful procedures, e.g.:
- Fracture reduction/manipulation
- Joint dislocation
- Suturing
- Incision and drainage of abscess
- Facilitation of femoral/fascia iliaca block for femoral fracture. In this setting ketamine may even be used to facilitate patient transfer into traction
- Insertion of tube thoracostomy
- Foreign body removal
- In paediatric procedural sedation, ketamine alone has been shown to be safer than ketamine in conjunction with fentanyl, ketamine in conjunction with midazolam, and ketamine in conjunction with propofol. Ketamine alone is also safer than propofol alone, and propofol in conjunction with fentanyl.
- Side effects of ketamine:
- Agitation (20%)
- Hypersalivation and lacrimation (<10%). Co-administration of atropine is not required.
- Vomiting (5-10%)
- Transient rash (10%)
- Involuntary movements/ataxia (5%)
- Serious adverse events of ketamine:
- Apnoea (0.3%). Usually due to rapid bolusing of ketamine. Slower IV administration over 60 seconds reduces the risk. May require airway repositioning or BVM ventilation.
- Airway misalignment/noisy breathing (1%). Basic airway repositioning usually sufficient to resolve this
- Laryngospasm (0.3%). Risk appears to be higher in children who undergo stimulation of posterior pharynx (e.g. deep oral cavity suturing) and children with URTI. Airway repositioning and BVM ventilation usually suffice in most cases. Reported incidence of intubation with laryngospasm is 0.02% (1 in 5000). See section on management of laryngospasm.
- Emergence phenomenon. Ketamine can induce agitation and hallucinations as dissociative effects wear off. Uncommon in children under 10 years old (1.6%), but more common beyond mid-adolescence (1 in 3 in adults). Can be managed with benzodiazepines on occurrence, but prophylactic benzodiazepines are not required.
Patient Selection
- Patients with ASA status I and II are appropriate candidates for procedural sedation in ED.
- Patients with an upper respiratory tract infection who are otherwise well can receive procedural sedation with ketamine in CED. However patients with a lower respiratory tract infection or an acute asthma attack should not receive procedural sedation with ketamine in CED.
|
ASA Class |
Description |
|
I |
Healthy, no underlying organic disease |
|
II |
Mild or moderate systemic disease that does not interfere with daily routines |
|
III |
Organic disease with definite functional impairment |
|
IV |
Severe disease that is life threatening |
|
V |
Moribund patient, not expected to survive |
|
E (suffix) |
Physical status classification appended with an “E” connotes a procedure undertaken as an emergency (e.g. an otherwise healthy patient presenting for fracture reduction is classified as ASA physical status I E) |
Pre-sedation Assessment
- Age and weight
- Fasting status
- It is important to note the fasting status of the patient (in case patient requires advanced airway management from airway complications of ketamine).
- However, a non-fasted status is NOT a contraindication to ketamine sedation.
- ASA status
- Pre-sedation level of consciousness
- Medical History:
- Airway: e.g., Obstructive sleep apnoea, large tonsils, airway malacia, current croup
- Respiratory: e.g., Asthma, bronchiectasis, cystic fibrosis
- Cardiac: e.g., Congenital heart disease (pre or post repair), congestive heart failure, arrhythmia
- Neurology: e.g., Seizure disorder, VP shunts, neuromuscular disease, cerebral palsy
- Psychiatric/developmental/behavioural: e.g., Autism spectrum disorder
- Others
- Current medications and allergies
- Previous anaesthetic and sedation history
- Physical examination
- Standard physical exam including cardiorespiratory, airway, level of consciousness
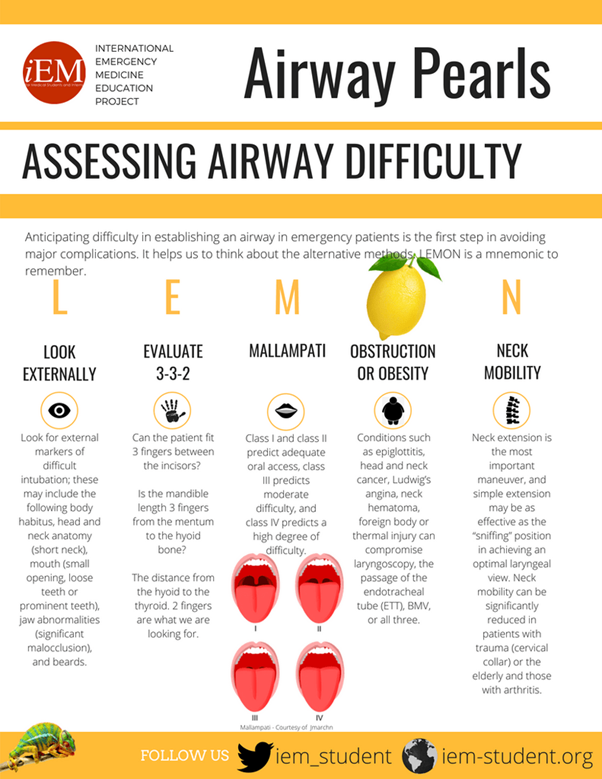
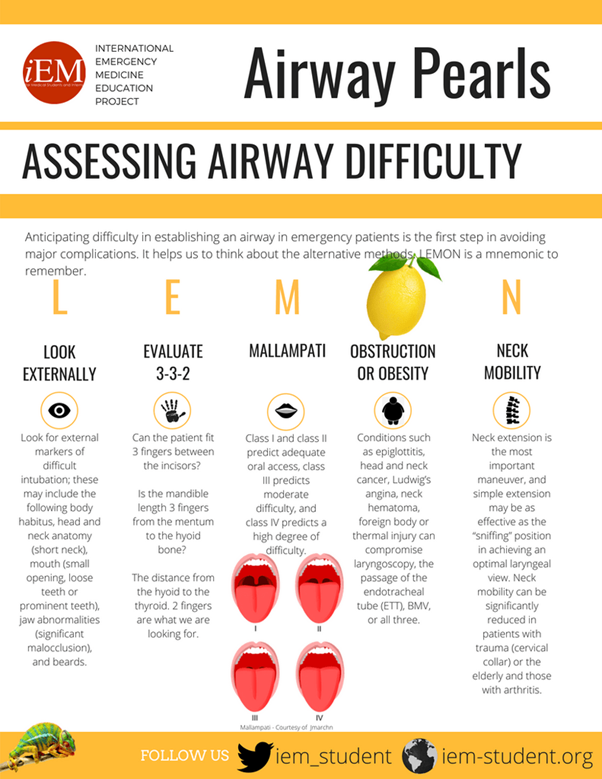
- LEMON is important. Please complete ALL component in LEMON in your pre-sedation assessment:
Informed Consent
- Informed verbal consent is required for ketamine. Please also provide ketamine advice sheet
- Drug to be used (ketamine) and method of administration (IV)
- Desired behaviour or expected response to sedation
- Expected duration and recovery period
- Possible adverse effects
- Possible alternatives to sedation (this is usually a formal GA in the operating theatre, for which the child will definitely require advanced airway managements)
Fasting status
- Children undertaking procedural sedation with ketamine does not need to be fasted.
- Research has shown no statistically nor clinically significant increase in adverse events in the unfasted patients.
- Cravero et al (2006) – in a series of over 30,000 children undergoing procedural sedation, only one episode of aspiration was reported (and this was in a fasted patient).
Personnel
At least 3 health care practitioner is required for procedural sedation with ketamine in CED:
- Proceduralist
- Sedationist and airway personnel: Usually CED registrar/NP/SMO
- Monitoring practitioner: Usually CED nurse
Checklist/Cheat Sheet Prior to Starting Ketamine Procedural Sedation in CED
- Pre-sedation assessment done and documented (in CED sedation sheet)
- CED SMO and nurse coordinator informed about sedation
- Informed verbal consent
- Required personnel all present
- Confirm correct patient by checking patient bracelet/with patient/with parent(s)
- Emergency resuscitation sheet by weight present (pre-printed ones are present in Procedure room 2, but please remember that endotracheal tube sizes should be AGE based, rather than weight based)
- Prefilled ketamine syringe (100mg/10mL)
- Emergency drugs present (in the “lunch box”)
- Confirm dose of paralytic drug (suxamethonium or rocuronium) by weight
- Check suction working
- Check oxygen supply working and confirm appropriately sized oxygen mask
- Prepare appropriately sized laryngoscope, endotracheal tube, laryngeal mask airway, oropharyngeal airway, bag valve mask ventilation device
- Ensure patient has appropriate monitoring present (3-lead cardiac monitoring and oxygen saturation monitoring)
Ketamine Dosing
- Initial intravenous dose: 1mg/kg IV given over 60 seconds
- Supplemental doses if required: 0.5mg/kg IV via slow push
Management of Complications
These are rare.
- Severe emergence phenomenon – If the patient is severely distressed, IV midazolam can be given in small incremental doses of 0.05mg/kg – 0.1mg/kg
- Intractable vomiting post procedure – consider use of IV ondansetron at a dose of 0.1mg/kg (up to 4mg) via slow IV push
- Laryngospasm
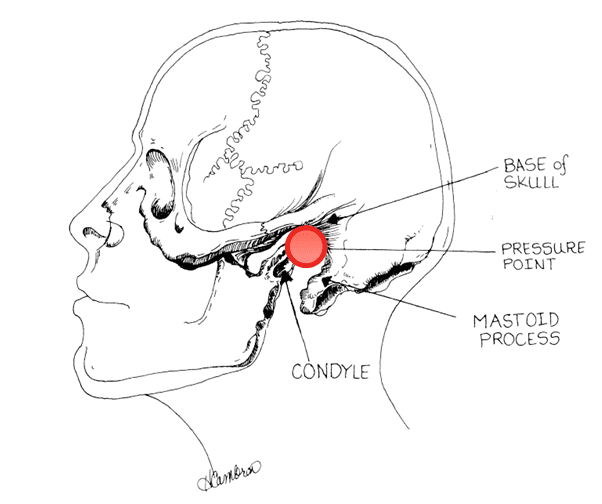
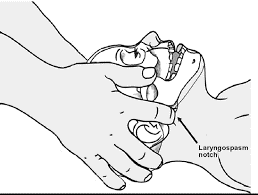
Larson’s manoeuvre: apply firm pressure on Larson’s point and simultaneously push forward similar to a jaw thrust manoeuvre. This causes pain over the styloid process and relaxes the cord.
Larson’s point is located behind the lobule of the pinna (of the ear), bounded anteriorly by the ascending ramus of the mandible adjacent to the condyle, posteriorly by the mastoid process of the temporal bone, and cephalad by the base of the skull.
Discharge Criteria
- Clearly defined discharge criteria can reduce time spent in recovery without compromising patient safety.
- Post sedation and during the recovery phase, the patient will be monitored by the nursing team based on current nursing monitoring guidelines in the CED.
- Patient can be discharged home when vital signs have returned to normal and he/she is awake with good control of protective reflexes.
References
- Cravero JP, Blike GT, Beach M, et al. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the Pediatric Sedation Research Consortium. Pediatrics. Sep 2006;118(3):1087-96. doi:10.1542/peds.2006-0313
- Bhatt M, Johnson DW, Chan J, et al. Risk Factors for Adverse Events in Emergency Department Procedural Sedation for Children. JAMA Pediatr. 10 2017;171(10):957-964. doi:10.1001/jamapediatrics.2017.2135
- Agrawal D, Manzi SF, Gupta R, Krauss B. Preprocedural fasting state and adverse events in children undergoing procedural sedation and analgesia in a pediatric emergency department. Ann Emerg Med. Nov 2003;42(5):636-46. doi:10.1016/s0196-0644(03)00516-x
- Hampson-Evans D, Morgan P, Farrar M. Pediatric laryngospasm. Paediatr Anaesth. Apr 2008;18(4):303-7. doi:10.1111/j.1460-9592.2008.02446.x
- Nickson C. Laryngospasm. Life in the Fast Lane. November 2020. https://litfl.com/laryngospasm/
- Assessing Airway Difficulty – LEMON. iEM. August 2018. https://iem-student.org/2018/08/01/assessing-airway-difficulty-lemon/
- Murphy M, Wall R. LEMON airway assessment method. The difficult and failed airway. In: Manual of Emergency Airway Management. Chicago, IL: Lippincott Williams and Wilkins;2001:31-39.
- The Royal College of Emergency Medicine. Best Practice Guideline: Ketamine Procedural Sedation for Children in the Emergency Department. 2020.
Ketamine Accreditation in Starship CED
Ketamine is a commonly used drug for procedural sedation in CED.
In order to achieve ketamine accreditation in CED, you will be required to complete these 2 components:
1. Complete the Ketamine Module: Please read the notes provided and complete the MCQ (link present at the end of the notes). You will need to achieve 8 or more correct answers (out of 10 questions) to pass this component. You can re-sit this MCQ as many times as you want – just remember to enter your email address and name prior to starting the MCQ.
2. Complete the Ketamine Sign-Off:
A. If you have previously achieved ketamine accreditation for procedural sedation in children (either in CED or in another emergency department), you are required to successfully pass these requirements:
· RACP trainees: Observe one ketamine sedation, then do one directly supervised ketamine sedation (supervised by SMO)
· ACEM trainees: one directly supervised ketamine sedation (supervised by SMO) done as a formal DOPS (direct observation of procedural skills)
B. If you have not previously achieved ketamine accreditation for procedural sedation in children, you are required to:
· Observe one ketamine sedation
· Do two directly supervised ketamine sedation (supervised by SMO)
· Do three indirectly supervised ketamine sedation (supervised by SMO)
The ketamine sign off sheet is located in Procedure room 2 in CED.
Introduction
- Ketamine is a synthetic phencyclidine derivative that causes a dissociative sedative state through binding with the NMDA (N-methyl-D-aspartate) receptor.
- Characteristics of ketamine “dissociative state”:
- Dissociation: trance-like state – eyes remain open, but patient does not respond
- Catalepsy: normal or slightly increased muscle tone; occasional muscular clonus may occur
- Anxiolysis
- Analgesia (substantial or complete)
- Amnesia (total)
- Maintenance of protective airway reflexes
- Cardiovascular stability: heart rate and blood pressure typically increase
- Nystagmus
- Dissociation from ketamine is either present or absent, with a narrow transition zone, and has no observable progression or depth, therefore further dosing does not cause deeper sedation.
- Ketamine has a wide margin of safety.
- The ketamine doses advised for procedural sedation are designed to leave the patient capable of maintaining their airway. There is a significant risk of failure of sedation if the procedure is prolonged. If a procedure is likely to be longer than 20 minutes, a general anaesthesia should be considered as an alternative.
- Ketamine onset:
- Clinical onset (approximately) 1 minute
- Effective sedation 10 – 20 minutes
- Time to discharge 90 minutes
- Ketamine should be used to facilitate short painful procedures, e.g.:
- Fracture reduction/manipulation
- Joint dislocation
- Suturing
- Incision and drainage of abscess
- Facilitation of femoral/fascia iliaca block for femoral fracture. In this setting ketamine may even be used to facilitate patient transfer into traction
- Insertion of tube thoracostomy
- Foreign body removal
- In paediatric procedural sedation, ketamine alone has been shown to be safer than ketamine in conjunction with fentanyl, ketamine in conjunction with midazolam, and ketamine in conjunction with propofol. Ketamine alone is also safer than propofol alone, and propofol in conjunction with fentanyl.
- Side effects of ketamine:
- Agitation (20%)
- Hypersalivation and lacrimation (<10%). Co-administration of atropine is not required.
- Vomiting (5-10%)
- Transient rash (10%)
- Involuntary movements/ataxia (5%)
- Serious adverse events of ketamine:
- Apnoea (0.3%). Usually due to rapid bolusing of ketamine. Slower IV administration over 60 seconds reduces the risk. May require airway repositioning or BVM ventilation.
- Airway misalignment/noisy breathing (1%). Basic airway repositioning usually sufficient to resolve this
- Laryngospasm (0.3%). Risk appears to be higher in children who undergo stimulation of posterior pharynx (e.g. deep oral cavity suturing) and children with URTI. Airway repositioning and BVM ventilation usually suffice in most cases. Reported incidence of intubation with laryngospasm is 0.02% (1 in 5000). See section on management of laryngospasm.
- Emergence phenomenon. Ketamine can induce agitation and hallucinations as dissociative effects wear off. Uncommon in children under 10 years old (1.6%), but more common beyond mid-adolescence (1 in 3 in adults). Can be managed with benzodiazepines on occurrence, but prophylactic benzodiazepines are not required.
Patient Selection
- Patients with ASA status I and II are appropriate candidates for procedural sedation in ED.
- Patients with an upper respiratory tract infection who are otherwise well can receive procedural sedation with ketamine in CED. However patients with a lower respiratory tract infection or an acute asthma attack should not receive procedural sedation with ketamine in CED.
|
ASA Class |
Description |
|
I |
Healthy, no underlying organic disease |
|
II |
Mild or moderate systemic disease that does not interfere with daily routines |
|
III |
Organic disease with definite functional impairment |
|
IV |
Severe disease that is life threatening |
|
V |
Moribund patient, not expected to survive |
|
E (suffix) |
Physical status classification appended with an “E” connotes a procedure undertaken as an emergency (e.g. an otherwise healthy patient presenting for fracture reduction is classified as ASA physical status I E) |
Pre-sedation Assessment
- Age and weight
- Fasting status
- It is important to note the fasting status of the patient (in case patient requires advanced airway management from airway complications of ketamine).
- However, a non-fasted status is NOT a contraindication to ketamine sedation.
- ASA status
- Pre-sedation level of consciousness
- Medical History:
- Airway: e.g., Obstructive sleep apnoea, large tonsils, airway malacia, current croup
- Respiratory: e.g., Asthma, bronchiectasis, cystic fibrosis
- Cardiac: e.g., Congenital heart disease (pre or post repair), congestive heart failure, arrhythmia
- Neurology: e.g., Seizure disorder, VP shunts, neuromuscular disease, cerebral palsy
- Psychiatric/developmental/behavioural: e.g., Autism spectrum disorder
- Others
- Current medications and allergies
- Previous anaesthetic and sedation history
- Physical examination
- Standard physical exam including cardiorespiratory, airway, level of consciousness
- LEMON is important. Please complete ALL component in LEMON in your pre-sedation assessment:
Informed Consent
- Informed verbal consent is required for ketamine. Please also provide ketamine advice sheet
- Drug to be used (ketamine) and method of administration (IV)
- Desired behaviour or expected response to sedation
- Expected duration and recovery period
- Possible adverse effects
- Possible alternatives to sedation (this is usually a formal GA in the operating theatre, for which the child will definitely require advanced airway managements)
Fasting status
- Children undertaking procedural sedation with ketamine does not need to be fasted.
- Research has shown no statistically nor clinically significant increase in adverse events in the unfasted patients.
- Cravero et al (2006) – in a series of over 30,000 children undergoing procedural sedation, only one episode of aspiration was reported (and this was in a fasted patient).
Personnel
At least 3 health care practitioner is required for procedural sedation with ketamine in CED:
- Proceduralist
- Sedationist and airway personnel: Usually CED registrar/NP/SMO
- Monitoring practitioner: Usually CED nurse
Checklist/Cheat Sheet Prior to Starting Ketamine Procedural Sedation in CED
- Pre-sedation assessment done and documented (in CED sedation sheet)
- CED SMO and nurse coordinator informed about sedation
- Informed verbal consent
- Required personnel all present
- Confirm correct patient by checking patient bracelet/with patient/with parent(s)
- Emergency resuscitation sheet by weight present (pre-printed ones are present in Procedure room 2, but please remember that endotracheal tube sizes should be AGE based, rather than weight based)
- Prefilled ketamine syringe (100mg/10mL)
- Emergency drugs present (in the “lunch box”)
- Confirm dose of paralytic drug (suxamethonium or rocuronium) by weight
- Check suction working
- Check oxygen supply working and confirm appropriately sized oxygen mask
- Prepare appropriately sized laryngoscope, endotracheal tube, laryngeal mask airway, oropharyngeal airway, bag valve mask ventilation device
- Ensure patient has appropriate monitoring present (3-lead cardiac monitoring and oxygen saturation monitoring)
Ketamine Dosing
- Initial intravenous dose: 1mg/kg IV given over 60 seconds
- Supplemental doses if required: 0.5mg/kg IV via slow push
Management of Complications
These are rare.
- Severe emergence phenomenon – If the patient is severely distressed, IV midazolam can be given in small incremental doses of 0.05mg/kg – 0.1mg/kg
- Intractable vomiting post procedure – consider use of IV ondansetron at a dose of 0.1mg/kg (up to 4mg) via slow IV push
- Laryngospasm
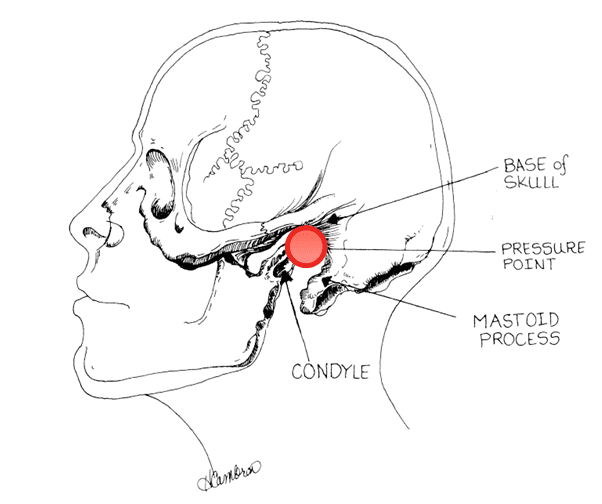
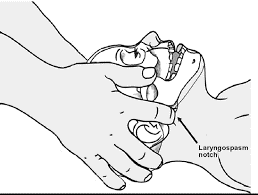
Larson’s manoeuvre: apply firm pressure on Larson’s point and simultaneously push forward similar to a jaw thrust manoeuvre. This causes pain over the styloid process and relaxes the cord.
Larson’s point is located behind the lobule of the pinna (of the ear), bounded anteriorly by the ascending ramus of the mandible adjacent to the condyle, posteriorly by the mastoid process of the temporal bone, and cephalad by the base of the skull.
Discharge Criteria
- Clearly defined discharge criteria can reduce time spent in recovery without compromising patient safety.
- Post sedation and during the recovery phase, the patient will be monitored by the nursing team based on current nursing monitoring guidelines in the CED.
- Patient can be discharged home when vital signs have returned to normal and he/she is awake with good control of protective reflexes.
References
- Cravero JP, Blike GT, Beach M, et al. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the Pediatric Sedation Research Consortium. Pediatrics. Sep 2006;118(3):1087-96. doi:10.1542/peds.2006-0313
- Bhatt M, Johnson DW, Chan J, et al. Risk Factors for Adverse Events in Emergency Department Procedural Sedation for Children. JAMA Pediatr. 10 2017;171(10):957-964. doi:10.1001/jamapediatrics.2017.2135
- Agrawal D, Manzi SF, Gupta R, Krauss B. Preprocedural fasting state and adverse events in children undergoing procedural sedation and analgesia in a pediatric emergency department. Ann Emerg Med. Nov 2003;42(5):636-46. doi:10.1016/s0196-0644(03)00516-x
- Hampson-Evans D, Morgan P, Farrar M. Pediatric laryngospasm. Paediatr Anaesth. Apr 2008;18(4):303-7. doi:10.1111/j.1460-9592.2008.02446.x
- Nickson C. Laryngospasm. Life in the Fast Lane. November 2020. https://litfl.com/laryngospasm/
- Assessing Airway Difficulty – LEMON. iEM. August 2018. https://iem-student.org/2018/08/01/assessing-airway-difficulty-lemon/
- Murphy M, Wall R. LEMON airway assessment method. The difficult and failed airway. In: Manual of Emergency Airway Management. Chicago, IL: Lippincott Williams and Wilkins;2001:31-39.
- The Royal College of Emergency Medicine. Best Practice Guideline: Ketamine Procedural Sedation for Children in the Emergency Department. 2020.